- Introduction:
Patient’s visit the dental clinic for a routine or planned visit for treatment, conditions related to the oral cavity or due to pain. Even with the invention of advanced dental techniques in restoration of teeth, extraction is one of the most routinely carried out dental procedure (El-Kenawy and Ahmed, 2015). Exodontia can be defined as “Painless removal of the whole tooth or tooth roots with minimal trauma to the investing tissues, so the wound heals un-eventfully” (Datarkar and Datarkar, 2007). Dental extraction procedures require a good understanding of anatomical structures along with adequate armamentarium and good technique. Successful treatment depends on good diagnosis, planning, appropriate surgical technique and well monitored post operative period. Even though it is a straight forward procedure, there is a possibility of complications during various stages of exodontia and the surgeon should be able to cope with it (Louis, 2015).
“Complications are unforeseen events that tend to increase the morbidity, above what would be expected from a particular operative procedure under normal circumstances” (Venkateshwar, et.al, 2011). They are rare and can arise due to a wide variety of factors. This report covers systemic and local complications for:
- Pre-operative
- Peri-operative
- Post-operative
-
Discussion:
-
Pre-operative complication and management
- Pre-operative Systemic complications:
-
Pre-operative complication and management
Pre-operative evaluation of the patient’s in-depth history (medical, dental or social) past and present and physical examination is crucial (Thakur, et.al, 2014). The patient should be asked about their chief complaint and history of present illness describing onset, quality, intensity, duration, location, radiation, exacerbating or relieving factors, medications (prescribed or over the counter) being taken including any allergies and the type of allergic response. A note of patient’s family history might reveal inherited illnesses such as haemophilia. Patient’s social support system should also be noted along with habits such as alcohol/drug intake and tobacco use.
A ROS should be completed and it might reveal undiagnosed medical conditions. Questionnaires are used for this purpose (Appendix 1). The common medical conditions and their management are discussed below:
- Cardiorespiratory: Angina, myocardial infarction, hypertension and asthma are most common. Symptoms are crushing chest pain, dyspnoea, oedema and palpitations. Patient’s will have difficulty in going up more than 20 stairs, also there is cough and wheeze. Minor treatment can be performed in case of stable angina, but elective dental care deferred in unstable or recent angina. The risk of MI in higher within the first 6 months of prior MI and are classified as ASA class IV and high risk procedures deferred. Elective dental care can be normally performed safely in asymptomatic patients with more than 12 months MI. Premedication is administered to patients having BP value between 160-190/95-110 mmHg (oral or inhalation sedation). There is no proof of cardiac risk reducing even in case of delaying surgery in patients who have BP higher than 180/110 mmHg (Andersson et al, 2010).
- Bleeding disorders: Questions should be asked about bleeding or bruising and family history. (Minimum platelet count for surgery 100,000 per micro litre). 5% tranexamic acid mouth wash given and patient on anticoagulants should have INR <2.5 for extraction.
- Endocrine disorders: Diabetes (Morning appointment 1- 1.5 hrs after breakfast, this avoids hypoglycaemic reaction), hyperthyroidism, hypothyroidism.
- Epileptic seizures: Type, frequency, precipitating factors.
- Allergies: Including local anaesthetics, antibiotics, analgesics, dental materials.
- Use of anticoagulants: INR of 2.0-3.5 is the safe range for performing simple exodontia procedures. The range is reduced to 1.6-1.9 for complicated procedures.
Bisphosphonates, Gastrointestinal disorders, Liver disorders and jaundice, Infections- HIV, hepatitis, syphilis or gonorrhoea, Pregnancy, Radiotherapy also need to be monitored as they could lead to complications. In all the above disorders the anxiety control protocol should be followed and pre-operative medications given if required. Physiological examination is also carried out to confirm dental or medical conditions along with the vital signs (Appendix 2). ASA classification for minimum pre-operative requirement is a protocol to be followed (Appendix 3).
- Pre-operative local complications:
- Pain: It can be odontogenic or non-odontogenic. Patient should be asked questions as explained in HOPI (2.1.1). It is treated based on WHO classification (Appendix 4)
- Infection: It can be a localised abscess or can spread into spaces (submandibular, sublingual or maxillary) adjoining the tooth causing severe complications as well as affect the use of anaesthetics during surgery. It is treated with the use of antibiotics (Yousuf, et.al, 2016).
- Peri-operative complications and their management:
2.2.1 Peri-operative Systemic complications:
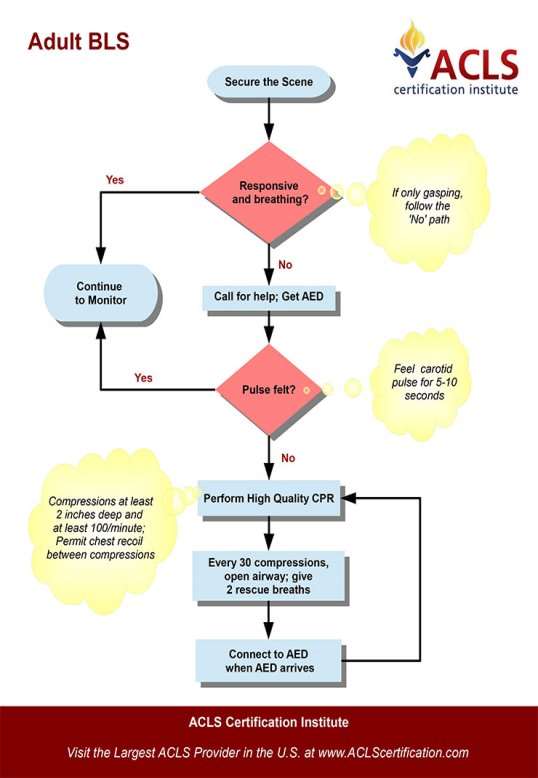
The following are the most commonly encountered conditions in dental practise (0.7 cases per dentist per year, Girdler, 1999). In the event of an attack, stay calm, stop dental treatment, make the environment safe, make patient sit upright in most cases, monitor vital signs, check for AVPU (Appendix 5) in conscious patient and follow ABCDE (Appendix 6) approach in unconscious patients (Scully,2014). In non-responding patients always call 999 and initiate CPR (Appendix 7). Emergency drugs and equipment list (Resuscitation council UK, 2013; Joshi & Acharya, 2016) (Appendix 8).
- Asthma: Few activations of patients own salbutamol inhaler (100 mcg/actuation) or 10 activations using large volume spacer device, repeated every 10 mins and oxygen (15 litres/min).
- Anaphylaxis: Give oxygen (15 litres/min), i.m adrenaline (anterolateral aspect of the middle third of vastus lateralis) in a dose 0.5 mL injection of 1:1000, repeated at 5 minute gap after monitoring vital signs. Paediatric dose given (Appendix 9).
- Angina: 2 GTN sprays (400 mcg/actuation) sublingually, oxygen (15 litres/min). Patient does not recover in 3 minutes treat for MI.
- MI: Call 999 immediately, sublingual GTN if not already given, single dose aspirin (300mg) orally to be chewed, oxygen (15litres/min).
- Epileptic seizures: Do not attempt to restrain movement, give oxygen (15litres/min), single dose of 10mg midazolam buccally.
- Hypoglycaemia: Conscious patient give oral glucose, repeated in 10 minutes. Unconscious patient give glucagon i.m route (1mg adults, 0.5mg children<8 years).
- Syncope: The patient should be laid flat immediately and legs elevated, give oxygen (15litres/min).
- Choking: Allow patient to cough vigorously, remove any visible foreign bodies, give 5 sharp back blows and if there is no dislodgement of the foreign body 5 abdominal thrusts are delivered (Heimlich) (Appendix 10).
2.2.2 Peri-operative Local complications:
These can be prevented by proper treatment planning, use of good surgical knowledge and technique. Pre-operative X-rays will help the dentist to locate any abnormalities in relation to the tooth and position of anatomical structures. Patient past dental history and blood test reports checked (Appendix 11). The experience of the surgeon plays a very important role in preventing these complications and effectively managing them.
- Soft tissue injuries: Due to improper manoeuvring or slippage of instruments. Common areas injured are lips, cheeks, palate, floor of mouth, tongue.
Management: Good flap reflection and luxation of tooth ensuring proper grip of instrument and soft tissue protection using thumb and forefinger of free hand. Small injuries need no treatment. In extensive injuries bleeding needs to be controlled and wound sutured.
- Tooth root fracture: Common event due to extensive caries, large restoration and endodontically treated tooth. Root tip fractures are common in posterior multirooted teeth. These are caused due to improper luxation and use of excessive forces using forceps.
Management: If root fracture is noted, irrigate socket thoroughly and directly visualise root. If root tip (<3mm) and no periapical pathology, there are chances of causing damage to adjacent anatomical structures, then it can be left in place. If there is associated pathology then the root elevators should be used to mobilise root fragment and then take it out.
- Crown fracture or luxation of adjacent tooth: Crown fracture (extensive caries or large restoration) and luxation of adjacent tooth occur when large amount of force is applied to extract a tooth using the adjacent tooth as fulcrum.
Management: Avulsed tooth repositioned and stabilised using splints for atleast 3-4 weeks. If there is any pain after this period the tooth needs to be restored with root canal treatment.
- Haemorrhage: Frequently occurs in most dental surgical procedures. It is mainly due to the trauma to the blood vessels or disorders of blood coagulation.
Management: Control bleeding and attempt to find the origin. Haemostasis obtained by Compression, Cellulose (Surgicel), Haemostatic Collagen (CollaPlug, CollaTape), Bone wax, 5% Tranexamic acid mouth wash, sutures and Electrocautery (Bagheri, et.al, 2016).
- Maxilla:
- Fracture of maxillary tuberosity: may create problem for denture retension and is because of extraction of the maxillary posterior teeth (bone weakened by maxillary sinus pneumatising into alveolar process), ankylosis of the tooth or decreased resistance of bone and poor technique (Von and Lozanoff,2017).
Management: If periosteum is not detached from the fractured segment, the bone is repositioned, tissue approximated, sutured and extraction rescheduled after 2 months. If bone segment completely reflected from tissues, tooth is first extracted, bone smoothened and wound sutured. Antibiotics with broad spectrum are prescribed.
- Displacement of tooth into maxillary sinus: Occurs when trying to luxate impacted maxillary third molar.
Management: Make the patient sit in upright position and take radiograph. If tooth is visible it can be removed by forcing positive pressure through sinus by closing nostril and exhaling. If this fails tooth can be removed by trephination using Caldwell-Luc (Appendix 12) or Lindorf approach (Boucree, et.al, 2015)
- Oroantral communication: Due to extraction of maxillary posterior teeth. It is confirmed from bubbling of blood from post extraction site when patient tries to breathe out while nostrils are pinched (Valslava test).
Management: small sized communication treated by filling alveolus with collagen and suturing using figure of 8 method. If tissues don’t approximate, portion of bone is removed to facilitate buccal and palatal tissue approximation. Large communications are treated using pedicle mucoperiosteal flaps. Antibiotics prescribed if tooth was infected along with nasal decongestants.
- Mandible:
- Fracture of mandible: associated with extraction of impacted third molars, due to excessive force applied by elevators or forceps, large pathologic lesions.
Management: If there is any fracture while extraction, tooth removal needs to be completed to prevent infection of the fracture line. Afterwards, case on case basis jaw segment stabilisation can be achieved by either intermaxillary fixation or rigid internal fixation for a period of upto 6 weeks. Administration of broad spectrum antibiotics is necessary.
- Dislocation of TMJ: Due to lengthy procedure on patients with TMJ disorders. There is mandibular deviation in the direction of the healthy side in unilateral dislocation, but there is prognathic movement of the mandible in bilateral dislocation. There is also restriction in mandibular movement and patients exhibit open bite. To prevent such problems mandible must be firmly supported in exodontia procedures.
Management: Thumbs placed on occlusal surfaces of teeth, the body of the mandible on both sides are supported by the other fingers. Thumbs are used to exert a downward pressure and at the same time the other fingers are used to push the mandible upwards and posteriorly, until condyle moves in its original position.
-
Post-operative complication & management:
- Post operative Local complication:
- Immediate- haemorrhage (2.2.2 d)
- Delayed-
Haemorrhage (2.2.2 d)
Swelling and pain (2.1.2)
Alveolar osteitis: Noticed couple of days after extraction due to blood clot disintegration resulting in necrosis in bone surface of the socket (Tong, et.al, 2014).
Management: Gentle irrigation of the wound area with saline and application of medicated packing to the area, e.g. eugenol dressings, and aggressive use of oral analgesics (Akinbami and Godspower, 2014).
- Late-
- Nerve injury: Inferior alveolar, mental, and lingual nerves. Nerve trauma may cause sensory disturbances (anesthesia, hypesthesia, paresthesia, dysesthesia) resulting in resulting in burning sensation, tingling, biting of tongue and lips, abnormal chewing. Nerve damage can be due to neurapraxia, axonotmesis, and neurotmesis.
Management: Usually palliative, painful situations require analgesics; also attempt is made to restore sensation using vitamin B complex. Often, the injured nerve segment needs to be replaced by using graft or suturing has to be performed on severed segments.
- Trismus: Masticatory muscle spasm causes restriction in mouth opening, normally with third molar extraction.
Management: Heat therapy, muscle relaxant medication, administration of analgesics, anti-inflammatory and physiotherapy lasting few minutes every 4 hours.
- Osteonecrosis: Can be due to MRONJ, 60% of patients had bone necrosis at extraction site. (Mansoor,2015; Heufelder,2014 ).
Management: Antibiotics prescribed to control infection. In advanced cases surgical removal of the necrotic bone is advised. Also microbial rinse along with daily irrigation can be done. Exposed bone can also be covered using a removable appliance.
Post Operative systemic complications are mainly related to haemolytic and haemorrhagic diseases and can be managed by using methods previously.
- Conclusion:
Exodontia is a simple procedure, practice of which inevitably can lead to complications from time to time. The complications arising due to these procedures can vary from a simple (dry socket) to the more complicated ones like everlasting nerve damage and displacement of tooth into maxillary sinus. There is a saying “prevention is better than cure” which is always best applied when trying to prevent the occurrence of these complications (Oliver, 2014). The surgeon should always be sure of patients past and present medical and dental history, make appropriate pre-operative tests and x-rays and formulate a treatment plan that is best for the patient.
Abbreviations:
- ABCDE – Airway, breathing, circulation, disability, exposure
- ASA – American Society of Anesthesiologists
- AVPU – Alert, voice, pain, unresponsive
- CPR – Cardiopulmonary resuscitation
- GTN – Glyceryl trinitrate
- HOPI – History of present illness
- i.m – Intramuscular
- INR – International normalised ratio
- MI – Myocardial infarction
- MRONJ – Medication-related osteonecrosis of jaws
- ROS – Review of systems
- TMJ – Temperomandibular joint
- WHO – World health organisation
References:
Akinbami, B.O. and Godspower, T., 2014. Dry Socket: incidence, clinical features, and predisposing factors. International journal of dentistry, 2014.
Bagheri, S.C., Bohluli, B. and Meyer, R.A., 2016. Oral surgery complications. Avoiding and Treating Dental Complications: Best Practices in Dentistry, p.103.
Boucree II, T.S. and Garri, J.I., 2015. Dental Extractions. In Ferraro’s Fundamentals of Maxillofacial Surgery (pp. 429-442). Springer New York.
Crispian Scully, 2014, medical problems in dentistry, Elsevier.
Datarkar, A.N. and Datarkar, A.N., 2007. Exodontia Practice. Jaypee Brothers Publishers.
Fragiskos D. Fragiskos , 2007, oral surgery, Springer.
Grandini, S.A., Barros, V.M., Salata, L.A., Rosa, A.L. and Soares, U.N., 1993. Complications in exodontia-Accidental dislodgment to adjacent anatomical areas. Braz Dent J, 3, p.103.
Heufelder M, 2014, Principles of oral surgery for prevention of bisphosphonate-related osteonecrosis of the jaw, Oral and Maxillofacial Surgery, Volume 117, Issue 6, June 2014, Pages e429-e435.
Joshi, S. and Acharya, S., 2016. Medical Emergencies in Dental Practice-A Nepalese study. Orthodontic Journal of Nepal, 5(2), pp.33-37.
Lars Andersson et al, 2010, Oral and maxillofacial surgery, Wiley-Blackwell
Louis, P.J., 2015. Complications of Dentoalveolar Surgery. Manual of Minor Oral Surgery for the General Dentist, p.265.
Mansoor, J., 2015. Pre-and postoperative management techniques. Before and after. Part 1: medical morbidities. British dental journal, 218(5), pp.273-278.
Mohamed H. El-Kenawy, Wael Moohamed Said Ahmed, 2015- comparison between physics and conventional forceps in simple dental extraction.
Oliver, R., 2014. Prevention and management of oral surgery complications in general dental practice. British dental journal, 216(5), pp.263-264.
Renton, T., Woolcombe, S., Taylor, T. and Hill, C.M., 2013. Oral surgery: part 1. Introduction and the management of the medically compromised patient. British dental journal, 215(5), pp.213-223.
Resuscitation council UK, 2013, medical emergencies and resuscitation,
www.resus.org.uk
Thakur, A.R., Babshet, M., Amur, S. and Naikmasur, V.G., 2014. Medical screening of dental patients: 16-year experience in a referral dental hospital. Journal of Medicine and the Person, 12(2), pp.76-83.
Tong, D.C., Al-Hassiny, H.H., Ain, A.B. and Broadbent, J.M., 2014. Post-operative complications following dental extractions at the School of Dentistry, University of Otago. New Zealand Dental Journal, 110(2).
Venkateshwar, G.P., Padhye, M.N., Khosla, A.R. and Kakkar, S.T., 2011. Complications of exodontia: a retrospective study. Indian journal of dental research, 22(5), p.633.
von Arx, T. and Lozanoff, S., 2017. Posterior Maxilla. In Clinical Oral Anatomy (pp. 133-162). Springer International Publishing.
Yousuf, W., Khan, M., Mehdi, H. and Mateen, S., 2016. Necessity of Antibiotics following Simple Exodontia. Scientifica, 2016.
Appendix: 1
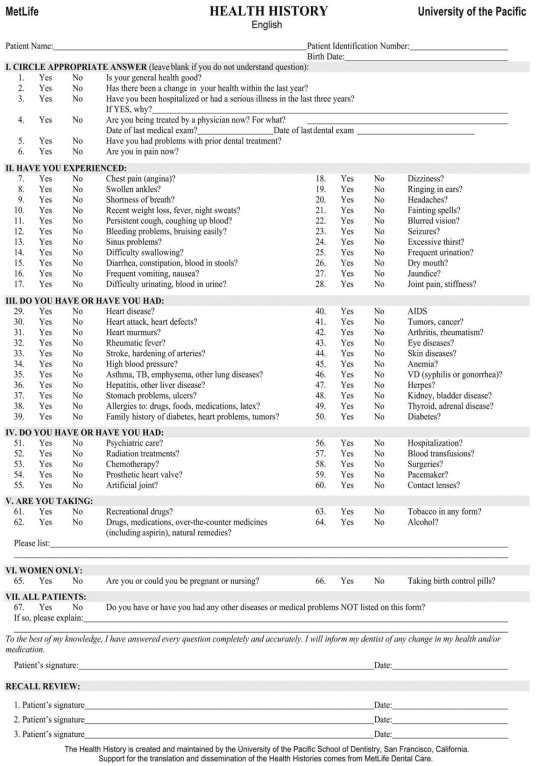
pocketdentistry.com
Appendix: 2
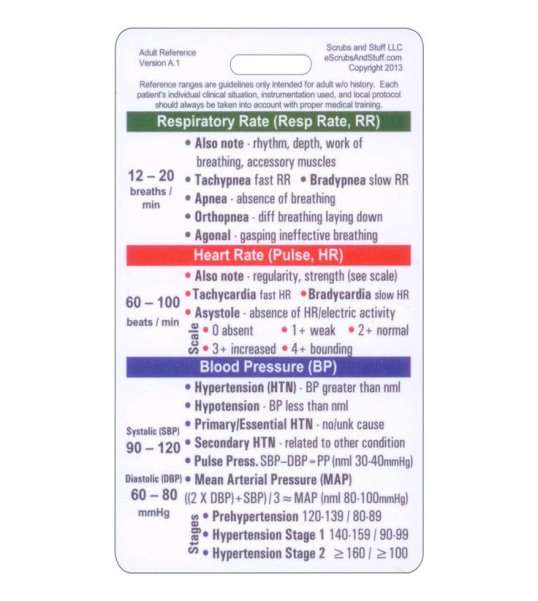
pocketdentistry.com
Appendix: 3
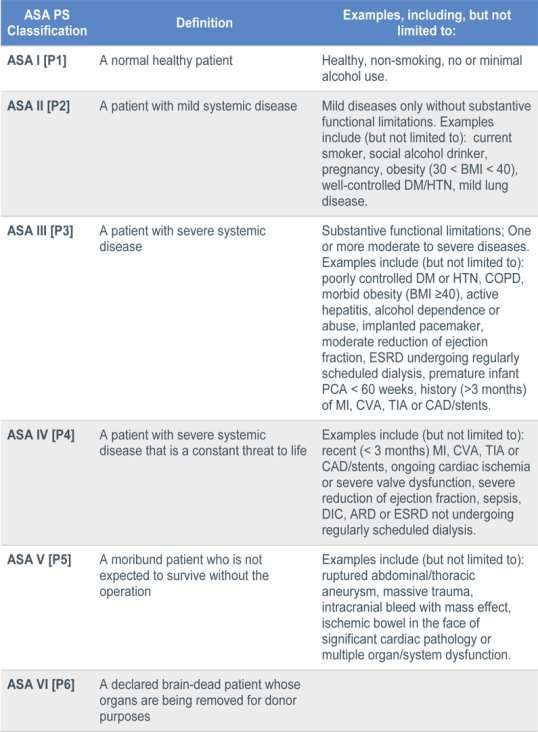
anesthesiallc.com
Appendix: 4
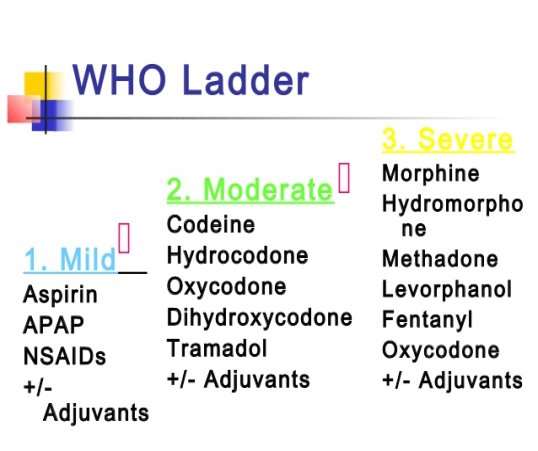
img.medscape.com
Appendix: 5
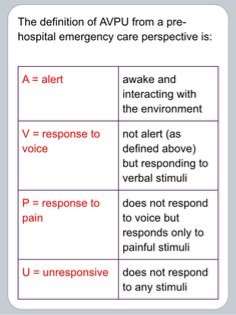
pocketdentistry.com
Appendix: 6
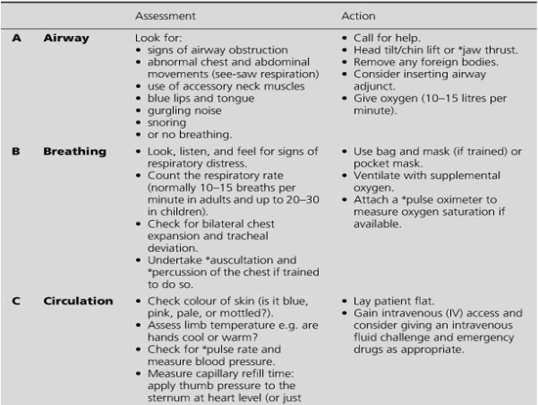
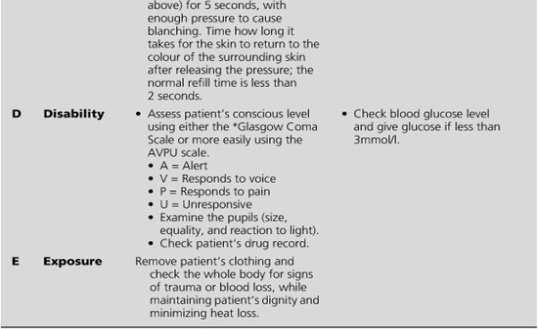
pocketdentistry.com
Appendix: 7
Appendix:8
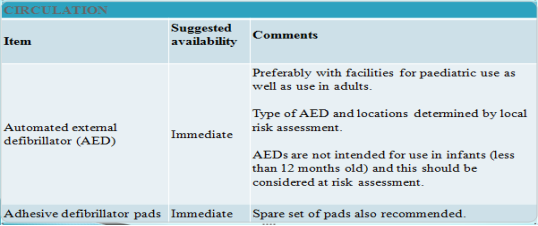
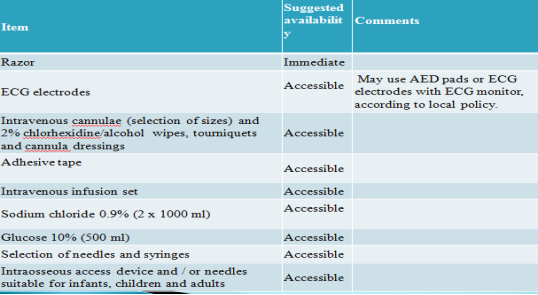
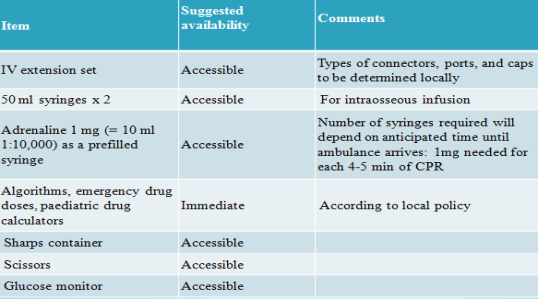
resus.org.u
Appendix: 9
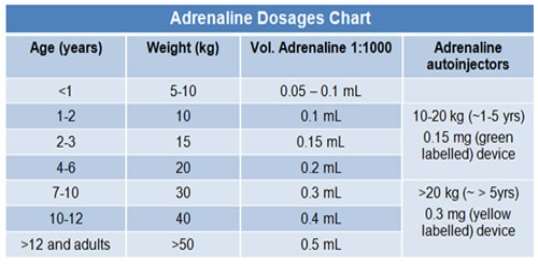
allergy.org
Appendix: 10
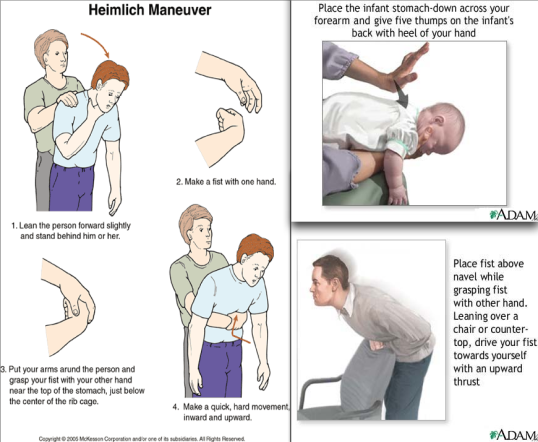
4.bp.blogspot.com
Appendix: 11
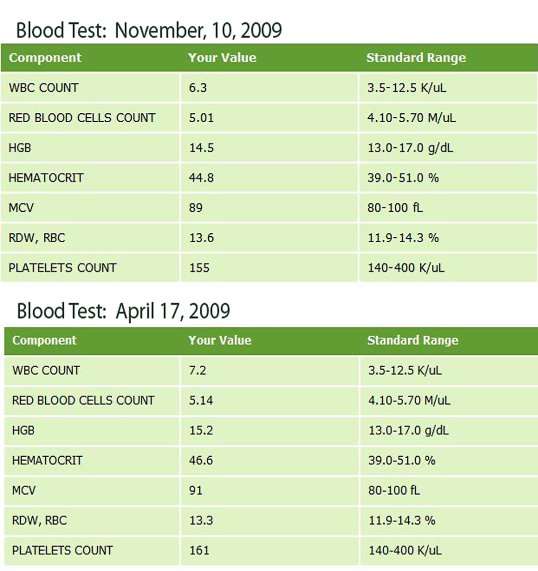
cllhealed.files.wordpress.com
Appendix: 12
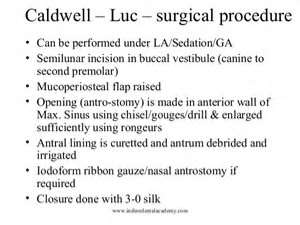
image.slidesharecdn.com
PLACE THIS ORDER OR A SIMILAR ORDER WITH NURSING TERM PAPERS TODAY AND GET AN AMAZING DISCOUNT

